Non-antibiotics with antibacterial properties pose a unique challenge to the standard understanding of drug interactions within the human body. Recent research by Noto Guillen et al. delved into this phenomenon, highlighting the potential for non-antibiotics to inadvertently disrupt the delicate balance of the gut microbiota with their unintended antimicrobial effects. By screening a variety of non-antibiotic drugs, the study revealed a significant divergence in the bacterial pathways targeted by these compounds compared to traditional antibiotics.
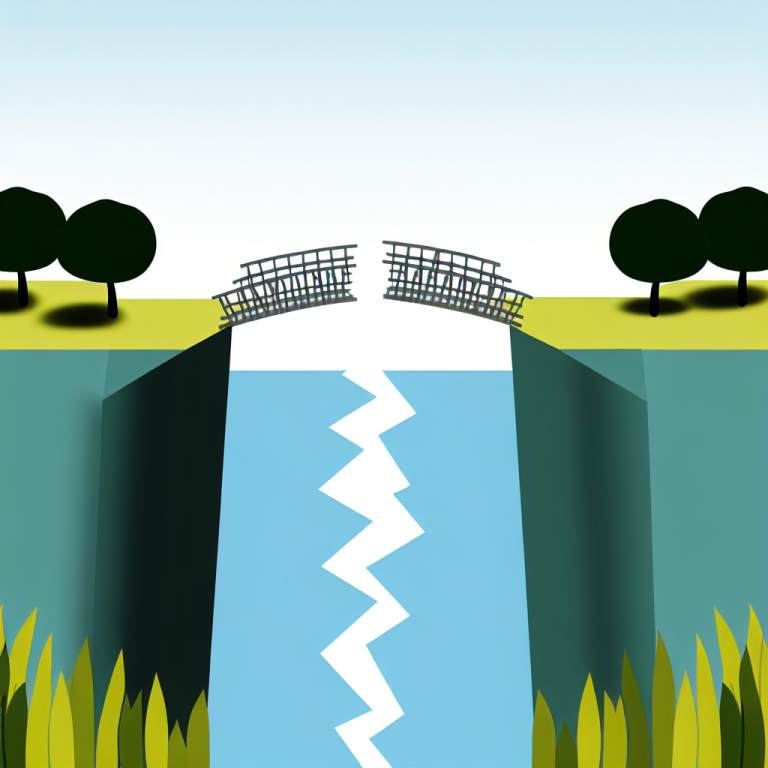
The analysis conducted by the research team identified patterns in the mode of action of antibiotics, which clustered by expected mechanisms, and non-antibiotics, which tended to affect divergent bacterial pathways. This network-based analysis not only shed light on the underlying source of side effects associated with long-term use of certain drugs, but also uncovered new possibilities for identifying unexpected targets for future antibiotics, such as a bacterial translation initiation factor.
Among the key findings was the revelation that non-antibiotics, including psychotropic agents, could potentially contribute to the development of antibiotic resistance through their impact on efflux systems. This highlights the crucial need to closely investigate the implications of non-antibiotics on antibiotic cross-resistance in real-life scenarios.
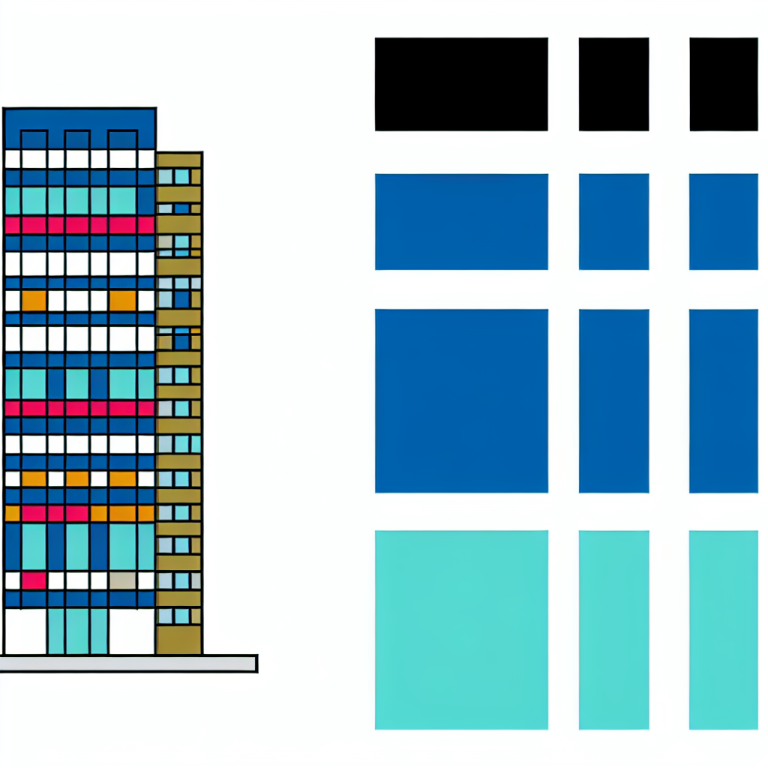
The study delved into the antibacterial activity of 200 drugs using genetic screens with barcoded Escherichia coli knockouts, unveiling over 2 million gene-drug interactions that underlie drug-specific toxicity. Notably, network-based analysis illustrated that antibiotics tended to cluster into modules corresponding to their established classes, while non-antibiotics remained disparate. This separation into distinct modules for non-antibiotics may offer novel insights into potential shared targets for new antimicrobials.
Moreover, the analysis of efflux systems revealed that these systems play a significant role in affecting the effectiveness of both antibiotics and non-antibiotics, emphasizing the importance of further studying how non-antibiotics can impact antibiotic cross-resistance.
The crucial role of the human microbiome in maintaining overall health and influencing the efficacy of various therapeutics cannot be understated. Studies have shown that numerous non-antibiotics can have a substantial impact on the human microbiome, potentially leading to dysbiosis. Shifts in microbiome composition have been associated with a variety of non-antibiotics, including antidiabetics, proton-pump inhibitors, antipsychotics, and nonsteroidal anti-inflammatory drugs.
It is becoming increasingly clear that the antibacterial activity of non-antibiotics at physiologically relevant concentrations warrants a deeper investigation into their mode of action in bacteria. The complexity of these interactions underscores the importance of understanding how various drugs – both traditional antibiotics and non-antibiotics – interact with the microbiome and potentially shape microbial populations in the body.
By uncovering the toxicity mechanisms of non-antibiotics and identifying shared and distinctive traits with standard antibiotic drug classes, researchers may pave the way for the development of novel antibiotics and address the potential challenges posed by unintended consequences of non-antibiotic use. The insights gained from this study may have far-reaching implications for future antibiotic development and antimicrobial resistance management strategies.