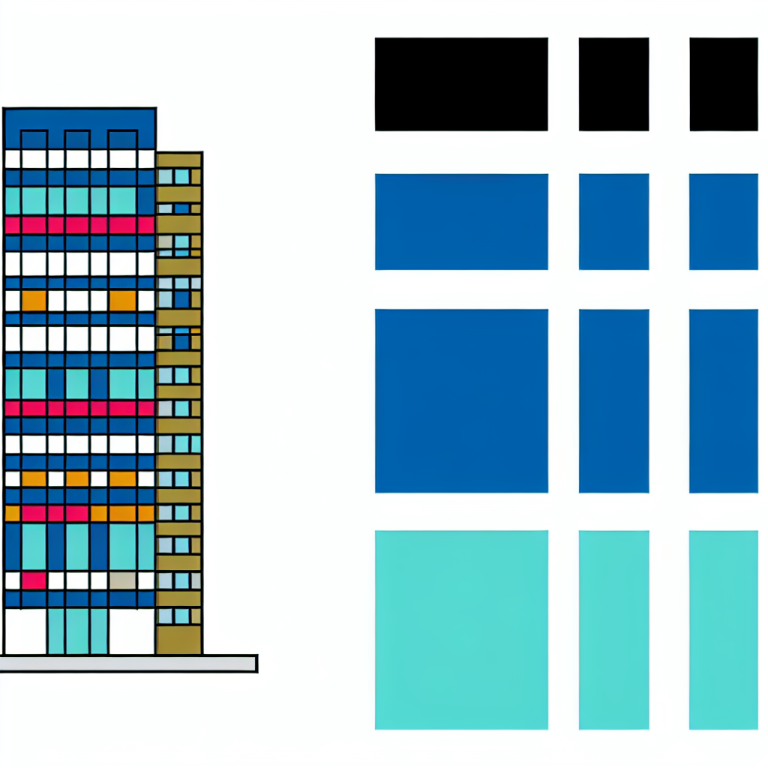
Nonantibiotic drugs have demonstrated potent antibacterial activity that can disrupt the human microbiome. The mechanisms behind this antibacterial activity remain largely unknown. To investigate this, a study was conducted where the antibacterial effects of 200 drugs were assessed using genetic screens with barcoded Escherichia coli knockouts. Through this analysis, researchers uncovered 2 million gene-drug interactions that contribute to drug-specific toxicity. It was observed that antibiotics fell into categorized modules based on their mode of action, while nonantibiotics did not directly correlate to any specific module. This separation suggests that nonantibiotics may offer untapped opportunities for the development of new antimicrobials.
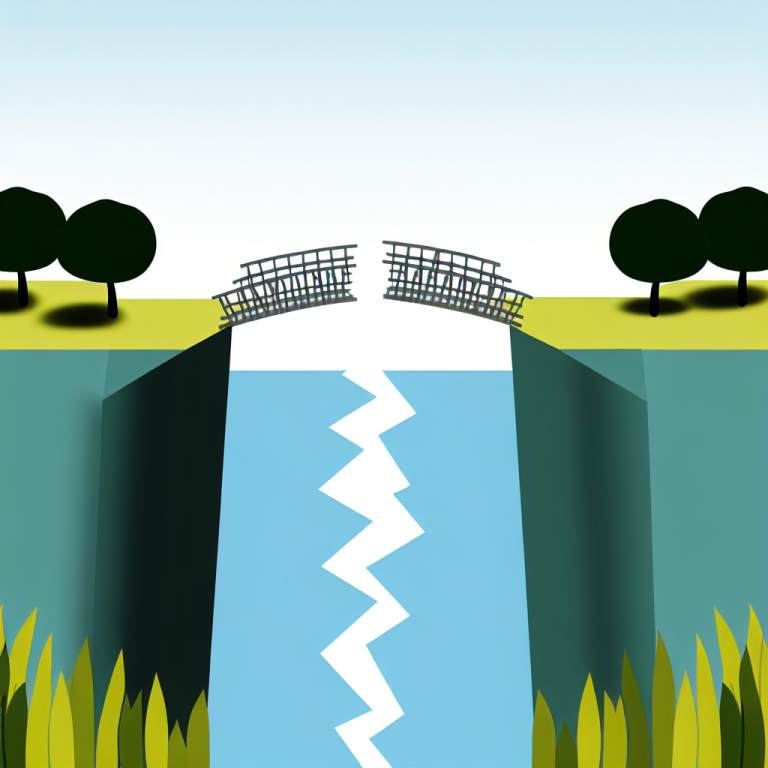
Efflux systems were also analyzed in the study and were found to impact antibiotics and nonantibiotics alike. This suggests that the impact of nonantibiotics on antibiotic resistance should be carefully studied in real-life scenarios. The human microbiome plays a crucial role in overall health and can influence the effectiveness of various treatments. Studies have shown that nonantibiotics, pharmaceutical drugs not typically used for bacterial infections, can be influenced by interactions with the microbiome.
Examples of nonantibiotics that have been associated with changes in microbiome composition include antidiabetic drugs, proton pump inhibitors, antipsychotics, and nonsteroidal anti-inflammatory drugs. The mechanisms driving these changes are complex, with direct interactions between the drugs and bacteria believed to play a significant role. Recent research has revealed that a significant number of nonantibiotics possess strong antibacterial properties at concentrations relevant to the human body.
The identification of these antibacterial properties raises questions about the exact mechanisms by which nonantibiotics impact bacteria. By studying a diverse panel of nonantibiotics, researchers aim to uncover common and unique toxicity mechanisms compared to traditional antibiotics. This information can help identify potential new targets for antibiotic development and highlight drugs that may inadvertently promote drug resistance when administered over extended periods.
The study utilized E. coli as a model to investigate the pathways responsible for bacterial growth inhibition by nonantibiotics. Genetic screening of nearly 200 drugs yielded valuable insights into bacterial fitness and helped reveal the orthogonal toxicity mechanisms of nonantibiotics compared to antibiotics. Efflux system knockouts were found to increase sensitivity to both antibiotics and nonantibiotics, highlighting their importance in bacterial defense mechanisms.
Laboratory evolution experiments supported the findings of the study by demonstrating that resistance developed against nonantibiotics can lead to broader antibiotic cross-resistance. Additionally, a novel cellular target, bacterial translation initiation factor IF2, was identified as a potential target that is currently not exploited by standard antibiotics. These results underscore the importance of understanding the impact of nonantibiotics on bacterial resistance and the microbiome to ensure the efficacy of antibiotic treatments in the future.