In a groundbreaking development, scientists have discovered that an analysis of 1,500 blood proteins can help predict the risk of developing dementia up to 15 years before an official diagnosis. The findings, reported in the journal Nature Aging, represent a significant step forward in the quest for a tool that can detect Alzheimer’s disease and other forms of dementia at a very early, pre-symptomatic stage.
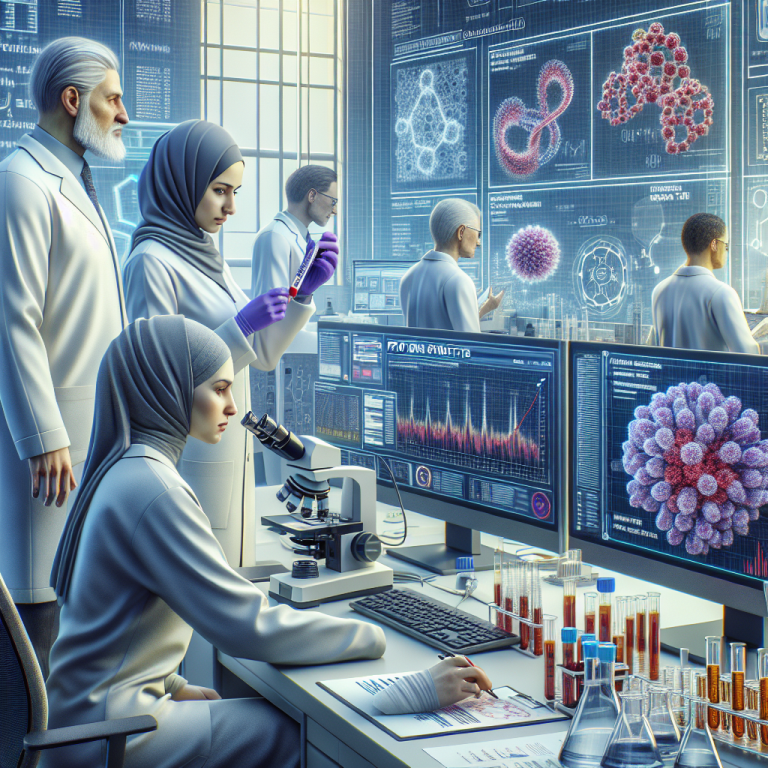
To conduct their study, researchers examined blood samples from over 50,000 healthy adults in the UK Biobank, 1,417 of whom went on to develop dementia over a period of 14 years. They found that high blood levels of four proteins – GFAP, NEFL, GDF15, and LTBP2 – were strongly associated with the development of dementia.
According to Amanda Heslegrave, a neuroscientist at University College London, “Studies are required to intervene with disease-modifying therapies at the very earliest stage of dementia.” Late diagnosis is a significant issue in dementia cases, as people often only seek medical attention when they start experiencing memory problems or other noticeable symptoms. By this point, the disease may have already been progressing for several years, making it nearly impossible to reverse.
In screening the blood samples of 52,645 individuals for 1,463 proteins, the authors of the study discovered that increased levels of GFAP, NEFL, GDF15, and LTBP2 were associated with not only dementia but also Alzheimer’s disease. Importantly, participants who developed dementia exhibited abnormal levels of these proteins more than ten years before the onset of symptoms.
The protein GFAP, which provides structural support to nerve cells called astrocytes, has previously been proposed as a diagnostic marker for Alzheimer’s disease. GDF15, another protein identified in the study, has also shown promise as a potential biomarker. The latest research revealed that individuals with high levels of GFAP in their blood are more than twice as likely to develop dementia and nearly three times as likely to develop Alzheimer’s compared to those with normal levels.
To create predictive algorithms, the authors employed machine learning techniques and combined the levels of the four protein biomarkers with demographic factors such as age, sex, education level, and family history. The model was trained using data from two-thirds of the study participants and achieved an impressive 90% accuracy in predicting the incidence of dementia subtypes, including Alzheimer’s disease, using data collected more than ten years before an official diagnosis.
While the findings hold tremendous potential, the researchers caution that these new biomarkers require further validation before they can be used as clinical screening tools. Replication of the study’s results and additional research to identify biomarkers that can distinguish between different forms of dementia should be a priority, according to Heslegrave.
If validated, these findings could pave the way for the development of blood tests that can identify individuals at risk of developing dementia and enable early intervention strategies to combat the disease. As the number of people living with dementia continues to rise worldwide, advancements in early detection and treatment could have far-reaching implications for both patients and healthcare systems.